Q-1. Drug of choice in a pregnant and hypertensive lady
a) Enalpril
b) Verapamil
c) Alpha Methyldopa
d) Thiazide
Answer: Alpha Methyldopa
Explanation:
Commonly used antihypertensive medications in pregnancy:
Severe hypertension:
Hydralazine
Labetalol
Short-acting Nifedipine
Mild to moderate hypertension:
Methyldopa
Labetalol
Hydralazine
Long-acting Nifedipine
Important points:
Congenital malformations have been reported with the use of ACE inhibitors during the first trimester of pregnancy, while fetal and neonatal toxicity, death, and congenital anomalies have been reported with the use of ACE inhibitors during the second and third trimesters of pregnancy.
If the patient becomes pregnant, Enalapril should be discontinued as soon as possible. Enalapril is considered contraindicated during pregnancy.
Q-2. Drug not given in PCOD
a) Tamoxifen
b) Clomiphene
c) Oral contraceptive
d) Metformin
Answer: Tamoxifen
Explanation:
Management of PCOD (Polycystic ovarian disease):
Obesity:
Weight loss improves the endocrine profile
Metformin improves insulin resistance and modest wt loss
Menstrual irregularity:
Combined oral contraceptive pills
Progestogen (such as medroxy-progesterone acetate or dydrogesterone
Infertility:
Ovulation can be induced with the anti- estrogens; the treatment of first choice is clomiphene citrate.
Hyper-androgenism:
All combined oral contraceptive pills will reduce ovarian androgen secretion but the use of androgen receptor-blocking drugs will confer additional benefit.
Cyproterone acetate and other anti-androgens such as spironolactone can be given in addition to a combined oral contraceptive pills.
Q-3. Antihypertensive contra-indicated in pregnancy
a) Methyldopa
b) Labetalol
c) Nifedipine
d) Enalprilate
Answer: Enalprilate
Explanation:
Commonly used antihypertensive medications in pregnancy:
Severe hypertension:
Hydralazine
Labetalol
Short-acting Nifedipine
Mild to moderate hypertension:
Methyldopa
Labetalol
Hydralazine
Long-acting Nifedipine
Important points:
Congenital malformations have been reported with the use of ACE inhibitors during the first trimester of pregnancy, while fetal and neonatal toxicity, death, and congenital anomalies have been reported with the use of ACE inhibitors during the second and third trimesters of pregnancy.
If the patient becomes pregnant, Enalapril should be discontinued as soon as possible. Enalapril is considered contraindicated during pregnancy.
Q-4. Which of these is not a support of the uterus?
a) Urogenital diaphragm
b) Pelvic diaphragm
c) Perineal body
d) Recto-vaginal septum
Answer: Recto-vaginal septum
Explanation:
Primary support of the uterus:
Muscular or active support:
Pelvic diaphragm
Perineal body
Urogenital diaphragm
Fibro-muscular or mechanical support:
Uterine axis
Pubo-cervical ligament
Transverse cervical ligament of Mackenrodt
Utero-sacral ligament
Round ligament of uterus
Q-5. A couple came for emergency contraception on 5th day of unprotected sexual intercourse. She is 32 years old and P2L2. What would you advice?
a) Levo-norgesterol 0.75mg
b) Copper IUCD
c) High dose OCP
d) Ligate tubes
Answer: Copper IUCD
Explanation:
Emergency contraception, or post-coital contraception, refers to methods of contraception that can be used to prevent pregnancy in the first 5 days after sexual intercourse.
Emergency contraception or post-coital contraception:
Copper-bearing intrauterine devices (IUDs)
Emergency contraception pills (ECPs) – Levo-norgestrel and Ulipristal acetate
Combined oral contraceptive pills or the Yuzpe method
Important points:
As couple family is complete, a copper-bearing IUD is preferred and most effective form of emergency contraception.
When inserted within 5 days of unprotected intercourse, a copper-bearing IUD is over 99% effective in preventing pregnancy. This is the most effective form of emergency contraception available.
Q-6. Carbetocin dose for PPH is
a) 100 microgram IM
b) 50 microgram IV
c) 150 microgram IV
d) 200 microgram IV
Answer: 100 microgram IM
Explanation:
WHO has developed guidelines supporting the use of a uterotonic when the full package of active management of the third stage of labour is not practised, which can be either oxytocin, 10 IU administered parenterally, or misoprostol, 600 µg administered orally.
Important point:
Misoprostol has been widely recommended to prevent postpartum hemorrhage when other methods are not available.
Life-threatening hyperpyrexia has been reported following the use of misoprostol, 800 µg orally, after childbirth.
Carbetocin, a long-acting oxytocin agonist, appears to be a promising agent for the prevention of PPH. Recommended dose of Carbetocin is 100 microgram administered slowly over a minute.
Q-7. 35 Year old female with 6 weeks amenorrhea comes to emergency department with nausea, vomiting and abdominal pain. Her pulse is 100/min and BP is 90/60 mm Hg. On ultrasound a right 5X5 cm adnexal mass is seen. What is likely management?
a) Immediate laparoscopic surgery
b) Beta-HCG
c) Methotrexate
d) IV fluid
Answer: Immediate laparoscopic surgery
Explanation:
Laparoscopy has become the recommended approach in most cases of ectopic pregnancy unless a woman is hemo-dynamically unstable.
Laparotomy is usually reserved for patients who are hemo-dynamically unstable or for patients with cornual ectopic pregnancies.
Important points:
Treatment with methotrexate is an especially attractive option when the pregnancy is located on the cervix or ovary or in the interstitial or the cornual portion of the tube.
Surgical treatment in these cases is often associated with increased risk of hemorrhage.
Q-8. A 16 yr old girl was brought with primary amenorrhea. Her mother mentioned that she started developing breast at the age of 12. She was prescribed OCPs 2 yrs back by a doctor with no effect. She was having normal stature and was a football player. On examination breast was well developed (Tanner’s stage V) and pubic hair was minimal (Tanner’s stage I). What is the diagnosis?
a) Premature ovarian failure
b) Turner’s syndrome
c) Androgen Insensitivity
d) Mullerian agenesis
Answer: Androgen Insensitivity
Explanation:
Androgen Insensitivity syndrome:
X-linked recessive disorder
Karyotype XY
External genitalia look like female
Adequate breast development without axillary and pubic hair or minimal axillary and pubic hair
Primary amenorrhea and absent uterus, hence will not respond to OCPs
Testes are placed in either labia or inguinal canal, or are intra-abdominal
Important point:
Mullerian agenesis patients will also have primary amenorrhea & absent uterus (Hence will not respond to OCPs) but have normal well developed axillary and pubic hair.
Q-9. A lady with abdominal mass was investigated. She was found to have bilateral ovarian masses with smooth surface. On microscopy they revealed mucin secreting cells with signet ring shape. Diagnosis
a) Krukenberg tumor
b) Dysgerminoma
c) Primary Adenocarcinoma of the ovaries
d) Dermoid cyst
Answer: Krukenberg tumor
Explanation:
Krukenberg tumor is a metastatic signet ring cell adeno-carcinoma of the ovary.
Stomach is the primary site in most Krukenberg tumor cases (70%). Carcinomas of colon, appendix, and breast (mainly invasive lobular carcinoma) are the next most common primary sites.
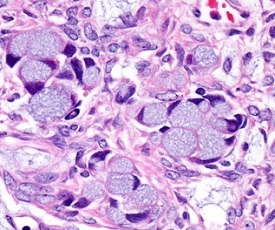
The tumor cells have abundant intracellular mucin and small crescentric hyper-chromatic atypical nuclei.
Q-10. According to the 2010 WHO criteria, what are the characteristics of normal semen analysis?
a) Volume 1.5 ml, count 15 million, morphology 4% progressive motility 32%
b) Volume 2.0 ml, count 20 million, morphology 4% progressive motility 32%
c) Volume 1.5 ml, count 20 million, morphology 4% progressive motility 32%
d) Volume 2.0 ml, count 15 million, morphology 40% progressive motility 32%
Answer: Volume 1.5 ml, count 15 million, morphology 4% progressive motility 32%
Explanation:
2010 WHO criteria: Characteristics of normal semen analysis
Parameter: WHO 2010
Volume: 1.5 ml
Concentration: 15 million/ml
Progressive motility: 32%
Normal forms: 4 %
Q-11. In severe preeclampsia, proteinuria level
a) 20 gm
b) 200 gm
c) 300 gm
d) 3000 gm
Answer: 300 gm
Explanation:
Significant protein excretion is defined as ≥ 300 mg in a 24-h urine collection or 1+ or greater on urine dipstick testing of two random urine samples that are collected at least 4 h apart.
Preeclampsia is defined by the new onset of elevated blood pressure and proteinuria after 20 weeks of gestation.
Important point:
According to the new ACOG guidelines, the diagnosis of preeclampsia no longer requires the detection of high levels of protein in the urine (proteinuria).
Q-12. A lady underwent vaginal hysterectomy for Ca cervix. Following the surgery after her urethral catheter was removed, she complained of urinary incontinence. On examination she had normal voiding as well as continuous incontinence. Methylene blue dye was instilled in her bladder through her urethra and she was given oral Phenazopyridine. After some time her pad was checked and it showed yellow staining at the top portion, but not the middle or bottom portions. She is likely to have
a) Uretero-vaginal fistula
b) Vesico-vaginal fistula
c) Urethro-vaginal fistula
d) Vesico-uterine fistula
Answer: Uretero-vaginal fistula
Explanation:
Three swab test:
Three swabs test is used to differentiate between uretero-vaginal fistula, Vesico-vaginal fistula and urethro-vaginal fistula.
Three cotton swabs are placed in the vagina – at the vault, in the middle and just above the introitus.
Methylene blue is introduced into the bladder using a rubber catheter.
Interpretation of three swab test:
Top swab soaked in urine, unstained – Uretero-vaginal fistula
Middle swab stained with dye – Vesico-vaginal fistula
Bottom swab stained with dye – Urethro-vaginal fistula
Double dye test:
It is useful for diagnosing Vesico-vaginal or uretero-vaginal fistulae.
For this test, the patient takes oral phenazopyridine and indigo carmine or methylene blue is filled into the empty urinary bladder via a urethral catheter.
Phenazopyridine turns urine orange in the kidneys, and methylene blue turns urine blue in the bladder.
A tampon is placed into the vagina. If the tampon turns blue, Vesico-vaginal fistula is suspected. If the tampon turns orange, uretero-vaginal fistula is suspected.
Q-13. A G6 + 0 + 0 lady with h/o recurrent missed abortion at 14-16wks, comes to you with a missed abortion. Which of the following tests is not warranted?
a) Lupus anticoagulant
b) Anti-cardiolipin ab
c) VDRL for wife and husband
d) Fetal Karyotype
Answer: VDRL for wife and husband
Explanation:
Causes and diagnosis of recurrent abortion:
Genetic error: Fetal and parental karyotyping
Anatomical abnormalities: Hysteroscopy or hystero-salpingogram
Hormonal abnormalities: T3 T4 and TSH, serum progesterone or endometrial biopsy during luteal phage and glucose tolerance test
Autoimmune diseases: Lupus anticoagulant and Anti-cardiolipin ab
Infection: Cervical culture
Q-14. What will be screened along with prolactin in Galactorrhea amenorrhea syndrome?
a) LH
b) TSH
c) HCG
d) Urine keto-acids
Answer: TSH
Explanation:
Patients with primary hypothyroidism have elevated TSH levels. TSH acts to stimulate the release of prolactin and may there by lead to Galactorrhea amenorrhea syndrome.
Q-15. A young girl with a mass in lower abdomen involving umbilical and hypogastric regions. On examination it is cystic and mobile and the examiner is unable to insinuate fingers between the mass and the pelvic bone. Likely diagnosis
a) Duplication of intestine
b) Mesenteric cyst
c) Omental cyst
d) Ovarian cyst
Answer: Ovarian cyst
Explanation:
Physical examination suggests pelvic mass. Correct answer is ovarian cyst.