Mondor’s disease is a rare, self-limiting entity characterised by subcutaneous chord like bands throughout the body. These bands arise due to phlebitis of the subcutaneous vessels. Penile Mondor’s disease (PMD) is an isolated superficial thrombophlebitis of the superficial dorsal vein of the penis. The exact pathophysiology is unknown, however it is frequently associated with prolonged or vigorous sexual intercourse. The disease is usually self-limiting and resolves with anti-inflammatory medications.
Definition
Henri Mondor (1885-1962) was a French physician and Professor of Clinical Surgery in Paris. He first described thrombophlebitis of the veins of the anterior chest wall in 1939 [1]. It was later in 1955 that Braun-Falco described dorsal phlebitis of the penis within the context of generalised phlebitis [2]. The first reported case of an isolated superficial thrombophlebitis of the dorsal vein of the penis was recorded by Helm and Hodge [3] in 1958 and subsequently defined as penile Mondor’s disease (PMD).
Incidence and epidemiology
PMD is rare and infrequently reported in the literature and as such the exact incidence is unknown. The real incidence of PMD could be greater than that reported due to the embarrassing nature of the complaint and its frequent spontaneous resolution. The largest case series in the literature reports on 25 cases [4]. PMD has been shown to affect sexually active men of any age (18-70 years) [5].
Aetiology
The exact cause of PMD remains unclear, but the most widely postulated theory is that it arises secondary to mechanical trauma. Case series document that patients frequently have a history of prolonged or vigorous sexual intercourse prior to the appearance of a lesion [6]. Usually lesions occur 24-48 hours following this sexual activity.
“Patients usually present with a palpable chord like lesion, which is always on the dorsum of the penis, arising 24-48 hours following vigorous or prolonged sexual intercourse.”
PMD has also been associated with sexually transmitted infections, however it is unclear whether the link is causal, or rather that increased sexual activity in this cohort is an incidental association [6]. Other causes linked to the onset of PMD are pelvic malignancy and recent groin or scrotal surgery (Table 1) [7].
Table 1:
Possible causes of penile Mondor’s disease [7].
Traumatic Prolonged or vigorous intercourse
Penile Trauma
Prolonged abstinence
Use of vacuum device
Infectious Syphilis
Candida infections
Sexually transmitted infections
Behcet’s disease
Surgical
Inguinal hernia repair
Orchidopexy
Varicoselectomy
Oncological
Pelvic malignancy
Other
Injection of intracavernous drugs
Tendency to thrombosis
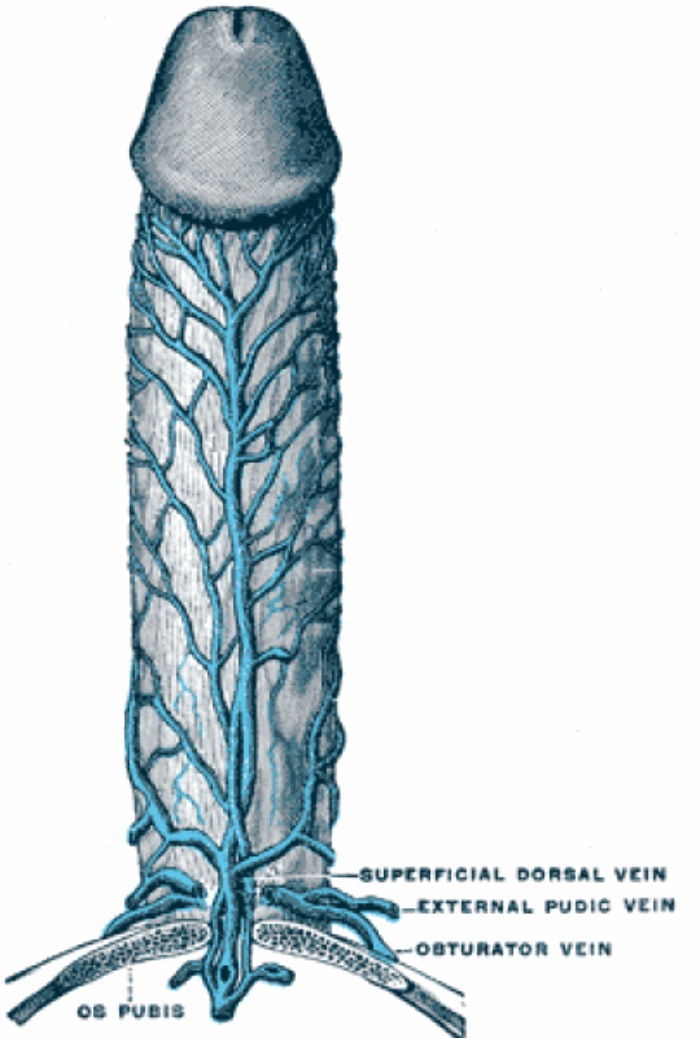
Figure1: The superficial dorsal vein of the penis starts distally draining the skin of the prepuce receiving numerous tributaries from the skin of the penis.
Pathology
The superficial dorsal vein of the penis starts distally draining the skin of the prepuce (Figure 1). It receives numerous tributaries from the skin of the penis as it courses proximally in the midline within the subcutaneous tissue of the penis, superficial to Buck’s fascia (Figure 2). It ultimately drains into the left and right superficial external pudendal veins, a tributary of the great saphenous vein.
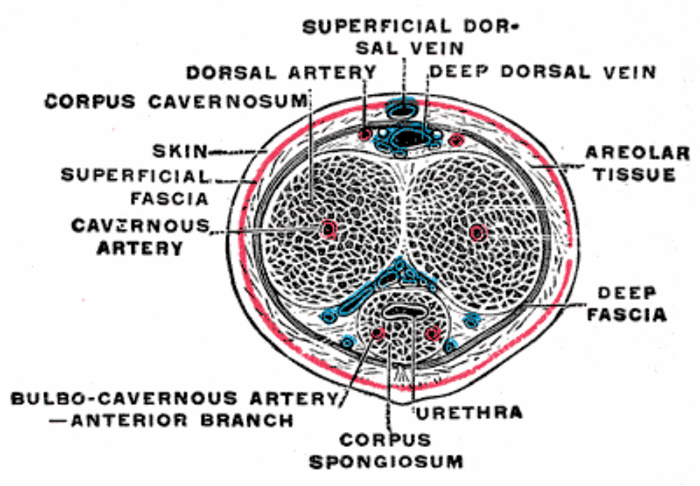
Figure 2: The superficial dorsal vein of the penis courses proximally in the midline within the subcutaneous tissue of the penis, superficial to Buck’s fascia.
In PMD histological analysis of resected thrombosed veins shows an increased amount of connective tissue in the vessel wall, with swelling of endothelial cells, and intraluminal thrombus. In the perivascular area an infiltration of lymphocytes, histiocytes and plasma cells can be seen [7].
Diagnosis
Patients usually present with a palpable chord like lesion, which is always on the dorsum of the penis, arising 24-48 hours following vigorous or prolonged sexual intercourse. The lesion can be tender and cause an episodic throbbing pain, which is exacerbated during erection. One case series reports up to a third of patients were asymptomatic [6].
On examination the lesion can be found on the dorsum of the penis, ranging between 2-10cm in length [7]. The overlying skin is tethered and sometimes erythematous. The chord like lesions can run longitudinally or transversely, and distal lesions can often give the appearance of a double coronal sulcus [6].
Good clinical examination and history can help differentiate PMD from the main differential of non-venereal sclerosing lymphangitis of the penis. This is another benign, self-limiting condition of the penis, which presents in sexually active men after vigorous sexual intercourse or masturbation. This condition instead, as its name suggests, affects the lymphatic system. It presents with similar subcutaneous cords, however these are non-tender and less extensive compared to PMD [8]. The two conditions can be differentiated formally by colour Doppler. Ultimately in most cases however, differentiating serves no clinical benefit as both conditions on the whole are treated conservatively.
Another differential diagnosis is Peyronie’s disease. A good clinical examination can differentiate whether the thickening is on the tunica albuginea or not.
Investigations
If investigation and formal diagnosis is required then colour Doppler ultrasound can be performed. In PMD signs of venous thrombosis are detected including no colour filling or flow in the lumen of the superficial dorsal vein associated with a low speed, high resistance flow pattern in the cavernous arteries [9]. Colour Doppler ultrasound is the key investigation in differentiating PMD from non-venereal sclerosing lymphangitis, which does not exhibit any of these features.
Bloods tests have little benefit in the work-up of PMD, and investigating for an increased tendency for thrombosis is rarely required [7].
Management
The management of PMD is entirely symptomatic. Patients can be managed expectantly with advice to abstain from sexual intercourse whilst they are symptomatic. Further to this patients often require strong reassurance of the benign nature and proper explanation.
In the literature patients are frequently given non-steroidal anti-inflammatories. These have been shown to be effective for treating the acute discomfort but had no effect on the rate of resolution [10]. Similarly, topical heparin creams have also been given showing no significant improvement in the rate of resolution [4].
There are cases of surgical intervention in cases refractory to medical treatment. Thrombectomy or resection of the dorsal vein of the penis can be performed. This is often offered to symptomatic patients failing to improve after six weeks [4].
Prognosis
PMD is a self-limiting condition, with most cases resolving within four to eight weeks [6,10]. Episodes of recurrence have been documented, which again have been associated with sexual intercourse [6,10].