aginal atrophy (atrophic vaginitis)
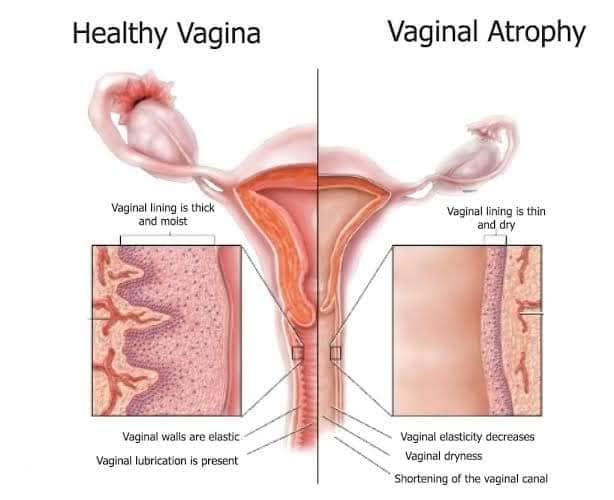
Vaginal atrophy (atrophic vaginitis) is thinning, drying and inflammation of the vaginal walls due to your body having less estrogen. Vaginal atrophy occurs most often after menopause.
For many women, vaginal atrophy not only makes intercourse painful, but also leads to distressing urinary symptoms. Because of the interconnected nature of the vaginal and urinary symptoms of this condition, experts agree that a more accurate term for vaginal atrophy and its accompanying symptoms is “genitourinary syndrome of menopause (GSM).”
Symptoms
With moderate to severe genitourinary syndrome of menopause (GSM), you may experience the following vaginal and urinary signs and symptoms:
Vaginal dryness
Vaginal burning
Vaginal discharge
Genital itching
Burning with urination
Urgency with urination
More urinary tract infections
Urinary incontinence
Light bleeding after intercourse
Discomfort with intercourse
Decreased vaginal lubrication during sexual activity
Shortening and tightening of the vaginal canal
Causes
Genitourinary syndrome of menopause (GSM) is caused by a decrease in estrogen production. Less estrogen makes your vaginal tissues thinner, drier, less elastic and more fragile.
A drop in estrogen levels may occur:
After menopause
During the years leading up to menopause (perimenopause)
After surgical removal of both ovaries (surgical menopause)
After pelvic radiation therapy for cancer
After chemotherapy for cancer
As a side effect of breast cancer hormonal treatment
GSM signs and symptoms may begin to bother you during the years leading up to menopause, or it may not become a problem until several years into menopause. Although the condition is common, not all menopausal women experience GSM. Regular sexual activity, with or without a partner, can help you maintain healthy vaginal tissues.
Risk factors
Certain factors may contribute to genitourinary syndrome of menopause (GSM), such as:
Smoking.
Cigarette smoking affects your blood circulation, resulting in the vagina and other tissues not getting enough oxygen. Smoking also reduces the effects of naturally occurring estrogens in your body. In addition, women who smoke typically experience an earlier menopause.
No vaginal births.
Researchers have observed that women who have never given birth vaginally are more likely to develop GSM than women who have had vaginal deliveries.
No sexual activity.
Sexual activity, with or without a partner, increases blood flow and makes your vaginal tissues more elastic.
Complications
Genitourinary syndrome of menopause (GSM) increases your risk of:
Vaginal infections.
Changes in the acid balance of your vagina makes vaginal infections (vaginitis) more likely.
Urinary problems.
Urinary changes associated with GSM can contribute to urinary problems. You might experience increased frequency or urgency of urination or burning with urination. Some women experience more urinary tract infections or incontinence.
DIAGNOSIS
Pelvic exam,
during which your doctor feels (palpates) your pelvic organs and visually examines your external genitalia, vagina and cervix. During the pelvic exam, your doctor also checks for signs of pelvic organ prolapse — indicated by bulges in your vaginal walls from pelvic organs such as your bladder or rectum or stretching of the support tissues of the uterus.
Urine test,
which involves collecting and analyzing your urine, if you have urinary symptoms.
Acid balance test,
which involves taking a sample of vaginal fluids or placing a paper indicator strip in your vagina to test its acid
Treatment
To treat genitourinary syndrome of menopause (GSM), your doctor may first recommend that you:
Try a vaginal moisturizer
restore some moisture to your vaginal area. You may have to apply the moisturizer every two to three days. The effects of a moisturizer generally last a little longer than those of a lubricant.
Use a water-based lubricant
(Astroglide, K-Y jelly, Sliquid, others) to reduce discomfort during intercourse. Choose products that don’t contain glycerin because women who are sensitive to this chemical may experience burning and irritation. Avoid petroleum jelly or other petroleum-based products for lubrication if you’re also using condoms. Petroleum can break down latex condoms on contact.Bothersome symptoms that don’t improve with over-the-counter treatments may be helped by:
Topical (vaginal) estrogen.
Vaginal estrogen has the advantage of being effective at lower doses and limiting your overall exposure to estrogen because less reaches your bloodstream. It may also provide better direct relief of symptoms than oral estrogen does.
Oral estrogen.
Estrogen taken by mouth enters your entire system. Ask your doctor to explain the risks vs. the benefits of oral estrogen.
Topical estrogen
Vaginal estrogen therapy comes in several forms. Because they all seem to work equally well, you and your doctor can decide which one is best for you.
Vaginal estrogen cream.
You insert this cream directly into your vagina with an applicator, usually at bedtime. Your doctor will let you know how much cream to use and how often to insert it. Typically women use it daily for one to three weeks and then one to three times a week thereafter. Although creams may offer faster relief than do other forms of vaginal estrogen, they can be messier.
Vaginal estrogen ring.
You or your doctor inserts a soft, flexible ring into the upper part of the vagina. The ring releases a consistent dose of estrogen while in place and needs to be replaced about every three months. Many women like the convenience this offers. A different, higher dose ring is considered a systemic rather than topical treatment.
Vaginal estrogen tablet.
You use a disposable applicator to place a vaginal estrogen tablet in your vagina. Your doctor will let you know how often to insert the tablet. You might, for instance, use it daily for the first two weeks and then twice a week thereafter.