Asthma is a common long term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. These episodes may occur a few times a day or a few times per week. Depending on the person they may become worse at night or with exercise.
Asthma is thought to be caused by a combination of genetic and environmental factors. Environmental factors include exposure to air pollution and allergens. Other potential triggers include medications such as aspirin and beta blockers. Diagnosis is usually based on the pattern of symptoms, response to therapy over time, and spirometry. Asthma is classified according to the frequency of symptoms, forced expiratory volume in one second (FEV1), and peak expiratory flow rate. It may also be classified as atopic or non-atopic where atopy refers to a predisposition toward developing a type 1 hypersensitivity reaction.
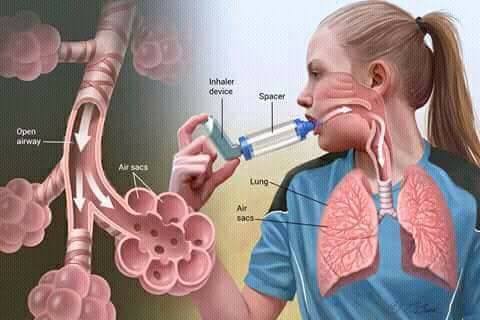
There is no cure for asthma. Symptoms can be prevented by avoiding triggers, such as allergens and irritants, and by the use of inhaled corticosteroids. Long-acting beta agonists (LABA) or antileukotriene agents may be used in addition to inhaled corticosteroids if asthma symptoms remain uncontrolled. Treatment of rapidly worsening symptoms is usually with an inhaled short-acting beta-2 agonist such as salbutamol and corticosteroids taken by mouth. In very severe cases, intravenous corticosteroids, magnesium sulfate, and hospitalization may be required.
Sign & Symptoms
According to the leading experts in asthma, the symptoms of asthma and best treatment for you or your child may be quite different than for someone else with asthma.
The most common symptom is wheezing. This is a scratchy or whistling sound when you breathe. Other symptoms include:
Shortness of breathChest tightness or painChronic coughingTrouble sleeping due to coughing or wheezing
Asthma symptoms, also called asthma flare-ups or asthma attacks, are often caused by allergies and exposure to allergens such as pet dander, dust mites, pollen or mold. Non-allergic triggers include smoke, pollution or cold air or changes in weather.
Asthma symptoms may be worse during exercise, when you have a cold or during times of high stress.
Children with asthma may show the same symptoms as adults with asthma: coughing, wheezing and shortness of breath. In some children chronic cough may be the only symptom.
If your child has one or more of these common symptoms, make an appointment with an allergist / immunologist:
Coughing that is constant or that is made worse by viral infections, happens while your child is asleep, or is triggered by exercise and cold airWheezing or whistling sound when your child exhalesShortness of breath or rapid breathing, which may be associated with exerciseChest tightness (a young child may say that his chest “hurts” or “feels funny”)Fatigue (your child may slow down or stop playing)Problems feeding or grunting during feeding (infants)Avoiding sports or social activitiesProblems sleeping due to coughing or difficulty breathing
Patterns in asthma symptoms are important and can help your doctor make a diagnosis. Pay attention to when symptoms occur:
At night or early morningDuring or after exerciseDuring certain seasonsAfter laughing or cryingWhen exposed to common asthma triggersCauses
It isn’t clear why some people get asthma and others don’t, but it’s probably due to a combination of environmental and genetic (inherited) factors.
Asthma triggers
Exposure to various irritants and substances that trigger allergies (allergens) can trigger signs and symptoms of asthma. Asthma triggers are different from person to person and can include:
Airborne substances, such as pollen, dust mites, mold spores, pet dander or particles of cockroach wasteRespiratory infections, such as the common coldPhysical activity (exercise-induced asthma)Cold airAir pollutants and irritants, such as smokeCertain medications, including beta blockers, aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen (Aleve)Strong emotions and stressSulfites and preservatives added to some types of foods and beverages, including shrimp, dried fruit, processed potatoes, beer and wineGastroesophageal reflux disease (GERD), a condition in which stomach acids back up into your throatDiagnosis
An allergist diagnoses asthma by taking a thorough medical history and performing breathing tests to measure how well your lungs work.
One of these tests is called spirometry. You will take a deep breath and blow into a sensor to measure the amount of air your lungs can hold and the speed of the air you inhale or exhale. This test diagnoses asthma severity and measures how well treatment is working.
Many people with asthma also have allergies, so your doctor may perform allergy testing. Treating the underlying allergic triggers for your asthma will help you avoid asthma symptoms.
Treatment
The right medications for you depend on a number of things — your age, symptoms, asthma triggers and what works best to keep your asthma under control.
Preventive, long-term control medications reduce the inflammation in your airways that leads to symptoms. Quick-relief inhalers (bronchodilators) quickly open swollen airways that are limiting breathing. In some cases, allergy medications are necessary.
Long-term asthma control medications, generally taken daily, are the cornerstone of asthma treatment. These medications keep asthma under control on a day-to-day basis and make it less likely you’ll have an asthma attack. Types of long-term control medications include:
Inhaled corticosteroids.These anti-inflammatory drugs include fluticasone (Flonase, Flovent HFA), budesonide (Pulmicort Flexhaler, Rhinocort), flunisolide (Aerospan HFA), ciclesonide (Alvesco, Omnaris, Zetonna), beclomethasone (Qnasl, Qvar), mometasone (Asmanex) and fluticasone furoate (Arnuity Ellipta).You may need to use these medications for several days to weeks before they reach their maximum benefit. Unlike oral corticosteroids, these corticosteroid medications have a relatively low risk of side effects and are generally safe for long-term use.Leukotriene modifiers.These oral medications — including montelukast (Singulair), zafirlukast (Accolate) and zileuton (Zyflo) — help relieve asthma symptoms for up to 24 hours.In rare cases, these medications have been linked to psychological reactions, such as agitation, aggression, hallucinations, depression and suicidal thinking. Seek medical advice right away for any unusual reaction.Long-acting beta agonists. These inhaled medications, which include salmeterol (Serevent) and formoterol (Foradil, Perforomist), open the airways.Some research shows that they may increase the risk of a severe asthma attack, so take them only in combination with an inhaled corticosteroid. And because these drugs can mask asthma deterioration, don’t use them for an acute asthma attack.Combination inhalers. These medications — such as fluticasone-salmeterol (Advair Diskus), budesonide-formoterol (Symbicort) and formoterol-mometasone (Dulera) — contain a long-acting beta agonist along with a corticosteroid. Because these combination inhalers contain long-acting beta agonists, they may increase your risk of having a severe asthma attack.Theophylline. Theophylline (Theo-24, Elixophyllin, others) is a daily pill that helps keep the airways open (bronchodilator) by relaxing the muscles around the airways. It’s not used as often now as in past years.
Quick-relief (rescue) medications are used as needed for rapid, short-term symptom relief during an asthma attack — or before exercise if your doctor recommends it. Types of quick-relief medications include:
Short-acting beta agonists.These inhaled, quick-relief bronchodilators act within minutes to rapidly ease symptoms during an asthma attack. They include albuterol (ProAir HFA, Ventolin HFA, others) and levalbuterol (Xopenex).Short-acting beta agonists can be taken using a portable, hand-held inhaler or a nebulizer — a machine that converts asthma medications to a fine mist — so that they can be inhaled through a face mask or a mouthpiece.Ipratropium (Atrovent). Like other bronchodilators, ipratropium acts quickly to immediately relax your airways, making it easier to breathe. Ipratropium is mostly used for emphysema and chronic bronchitis, but it’s sometimes used to treat asthma attacks.Oral and intravenous corticosteroids. These medications — which include prednisone and methylprednisolone — relieve airway inflammation caused by severe asthma. They can cause serious side effects when used long term, so they’re used only on a short-term basis to treat severe asthma symptoms.
If you have an asthma flare-up, a quick-relief inhaler can ease your symptoms right away. But if your long-term control medications are working properly, you shouldn’t need to use your quick-relief inhaler very often.
Keep a record of how many puffs you use each week. If you need to use your quick-relief inhaler more often than your doctor recommends, see your doctor. You probably need to adjust your long-term control medication.
Allergy medications may help if your asthma is triggered or worsened by allergies. These include:
Allergy shots (immunotherapy). Over time, allergy shots gradually reduce your immune system reaction to specific allergens. You generally receive shots once a week for a few months, then once a month for a period of three to five years.Omalizumab (Xolair). This medication, given as an injection every two to four weeks, is specifically for people who have allergies and severe asthma. It acts by altering the immune system.
Bronchial thermoplasty
This treatment — which isn’t widely available nor right for everyone — is used for severe asthma that doesn’t improve with inhaled corticosteroids or other long-term asthma medications.
Generally, over the span of three outpatient visits, bronchial thermoplasty heats the insides of the airways in the lungs with an electrode, reducing the smooth muscle inside the airways. This limits the ability of the airways to tighten, making breathing easier and possibly reducing asthma attacks.
Prevention
While there’s no way to prevent asthma, by working together, you and your doctor can design a step-by-step plan for living with your condition and preventing asthma attacks.
Follow your asthma action plan. With your doctor and health care team, write a detailed plan for taking medications and managing an asthma attack. Then be sure to follow your plan.Asthma is an ongoing condition that needs regular monitoring and treatment. Taking control of your treatment can make you feel more in control of your life in general.Get vaccinated for influenza and pneumonia. Staying current with vaccinations can prevent flu and pneumonia from triggering asthma flare-ups.Identify and avoid asthma triggers. A number of outdoor allergens and irritants — ranging from pollen and mold to cold air and air pollution — can trigger asthma attacks. Find out what causes or worsens your asthma, and take steps to avoid those triggers.Monitor your breathing. You may learn to recognize warning signs of an impending attack, such as slight coughing, wheezing or shortness of breath. But because your lung function may decrease before you notice any signs or symptoms, regularly measure and record your peak airflow with a home peak flow meter.Identify and treat attacks early. If you act quickly, you’re less likely to have a severe attack. You also won’t need as much medication to control your symptoms.When your peak flow measurements decrease and alert you to an oncoming attack, take your medication as instructed and immediately stop any activity that may have triggered the attack. If your symptoms don’t improve, get medical help as directed in your action plan.Take your medication as prescribed. Just because your asthma seems to be improving, don’t change anything without first talking to your doctor. It’s a good idea to bring your medications with you to each doctor visit, so your doctor can double-check that you’re using your medications correctly and taking the right dose.Pay attention to increasing quick-relief inhaler use. If you find yourself relying on your quick-relief inhaler, such as albuterol, your asthma isn’t under control. See your doctor about adjusting your treatment.