Piriformis syndrome (part 1)
Piriformis syndrome is a peripheral neuritis of the sciatic nerve caused by an abnormal condition of the piriformis muscle. It frequently goes unrecognized or is misdiagnosed in clinical settings. Piriformis syndrome can “masquerade” as other common somatic dysfunctions, such as intervertebral discitis, lumbar radiculopathy, primary sacral dysfunction, sacroiliitis, sciatica, and trochanteric bursitis.
More than 16% of all adult work disability evaluations and examinations are performed to rate the patient’s partial or total disability associated with chronic low back pain. It is estimated that at least 6% of patients who are diagnosed as having low back pain actually have piriformis syndrome.
Delay in diagnosing piriformis syndrome may lead to pathologic conditions of the sciatic nerve, chronic somatic dysfunction, and compensatory changes resulting in pain, paresthesia, hyperesthesia, and muscle weakness.The challenge for physicians is to recognize symptoms and signs that are unique to piriformis syndrome, enabling appropriate treatment in a timely manner.
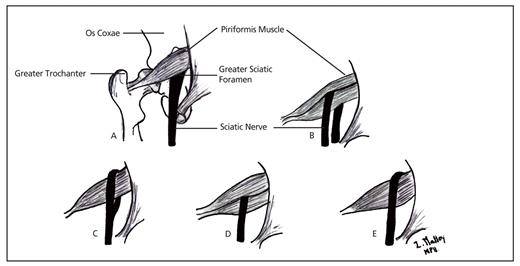
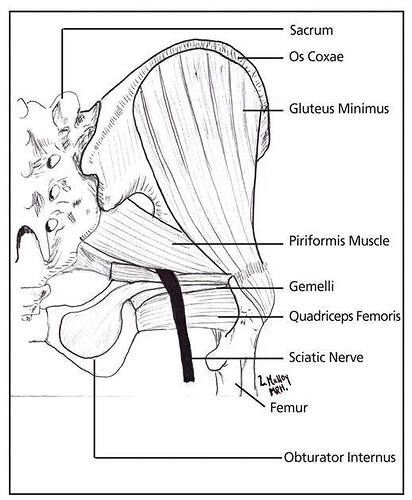
The proper understanding of piriformis syndrome requires knowledge of variations in the relationships between the sciatic nerve and the piriformis muscle . In as much as 96% of the population, the sciatic nerve exits the greater sciatic foramen deep along the inferior surface of the piriformis muscle.In as much as 22% of the population, the sciatic nerve pierces the piriformis muscle, splits the piriformis muscle, or both, predisposing these individuals to piriformis syndrome. The sciatic nerve may pass completely through the muscle belly, or the nerve may split—with one branch (usually the fibular portion) piercing the muscle and the other branch (usually the tibial portion) running inferiorly or superiorly along the muscle. Rarely, the sciatic nerve exits the greater sciatic foramen along the superior surface of the piriformis muscle.
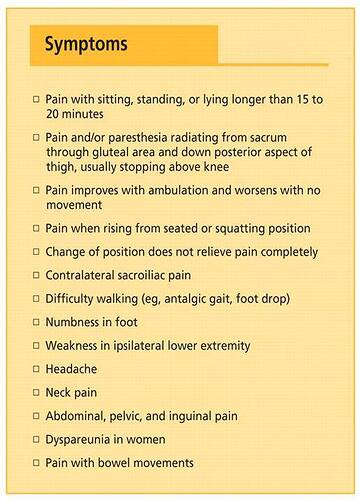
Some symptoms of piriformis syndrome occur as a result of local inflammation and congestion caused by the muscular compression of small nerves and vessels—including the pudendal nerve and blood vessels, which exit at the medial inferior border of the piriformis muscle.
he most common presenting symptom of patients with piriformis syndrome is increasing pain after sitting for longer than 15 to 20 minutes. Many patients complain of pain over the piriformis muscle (ie, in the buttocks), especially over the muscle’s attachments at the sacrum and medial greater trochanter. Symptoms, which may be of sudden or gradual onset, are usually associated with spasm of the piriformis muscle or compression of the sciatic nerve. Patients may complain of difficulty walking and of pain with internal rotation of the ipsilateral leg, such as occurs during cross-legged sitting or ambulation
Spasm of the piriformis muscle and sacral dysfunction (eg, torsion) cause stress on the sacrotuberous ligament. This stress may lead to compression of the pudendal nerves or increased mechanical stress on the innominate bones, potentially causing groin and pelvic pain. Compression of the fibular branch of the sciatic nerve often causes pain or paresthesia in the posterior thigh.
Through compensatory or facilitative mechanisms, piriformis syndrome may contribute to cervical, thoracic, and lumbosacral pain, as well as to gastrointestinal disorders and headache