Earlier in Fluid and Electrolyte disturbances, we talked about Sodium, Hyponatremia and Hyperkalemia. In this blog, potassium is going to be the target. Potassium is another mineral required in our body in minute amounts, yet it holds significant functions like resting cell membrane potential, hormone secretion, BP, glucose and insulin metabolism, renal concentrating abilitys, fluid-electrolyte balance, etc. However, even this small amount increases, causes hyperkalemia; if decreases, causes hypokalemia. Therefore, low potassium levels and high potassium levels are still not to be missed.
Normal Value and Physiology
Normal serum potassium concentration ranges between 3.5-5 mEq/L. Homeostasis of potassium balance is maintained through intake and renal excretion. It is mainly regulated by aldosterone. Aldosterone, diuretics (sodium delivery increased), osmotic diuretics (urine flow increased), high blood potassium levels, glucocorticoids and ADH (anti-diuretic hormone), all increase the renal excretion of potassium.
Upon increase of potassium levels, aldosterone-mediated mechanism increases excretion of potassium via kidney. Therefore, any factor which increases potassium uptake in cells, thereby increasing potassium levels, will increase its renal excretion via aldosterone.
Enhancers of potassium entry into cells: Insulin, Beta-adrenergic stimuli and Alkalosis
Factors decreasing potassium entry into cells: Glucagon, Alpha-adrenergic drugs and Acidosis
Hypokalemia
Hypokalemia is defined as low serum potassium levels going below 3.5 mEq/L. The mechanism included in hypokalemia are increased losses, decreased intake or transcellular shift.
Vomiting is a common cause of hypokalemia, which produces volume depletion and metabolic acidosis. On one hand, volume depletion initiates secondary hypoaldosteronism, which increases sodium resorption, therefore increasing potassium excretion. On other hand, metabolic acidosis also increases potassium excretion as there are less hydrogen ions for secretion in response to sodium resorption.
Causes
Following table lists the causes of hypokalemia, which includes Increased losses of Potassium, Decreased intake or stores of Potassium and Intracellular shift of Potassium from intracellular to extracellular.
HYPOKALEMIA CAUSES
Increased losses Renal loss: RTA (Renal tubular acidosis), Drugs like loop diuretics and thiazides, steroids, cystic fibrosis, giletman syndrome, bartter syndrome, liddle syndrome, mineralocorticoid excess (cushing syndrome, hyperaldosteronism, congenital adrenal hyperplasia), renin secreting tumors, renal artery stenosis
Extra-renal loss: Diarrhea, vomiting, sweating, potassium binding resins
Decreased intake or stores Malnutrition, anorexia nervosa; potassium-poor parenteral control
Intracellular shift Alkalosis, medications like beta-2 adrenergic agonists, theophylline, barium; refeeding syndrome, hypokalemic periodic paralysis, high insulin state, malignant hyperthermia, thyrotoxic periodic paralysis.
Signs and Symptoms
Hypokalemia or low potassium levels causes signs and symptoms which are related to muscular or cardiac functions. Severe hypokalemia, i.e, less than 2.5 mEq/L produces muscle weakness and cardiac arrythmia.
Diagnosis
Low potassium levels are further assessed using a ratio component called TTKG or Trans-tubular potassium gradient. It is calculated as :-
TTKG = (urine potassium x serum osmolality) / (serum potassium x urine osmolality)
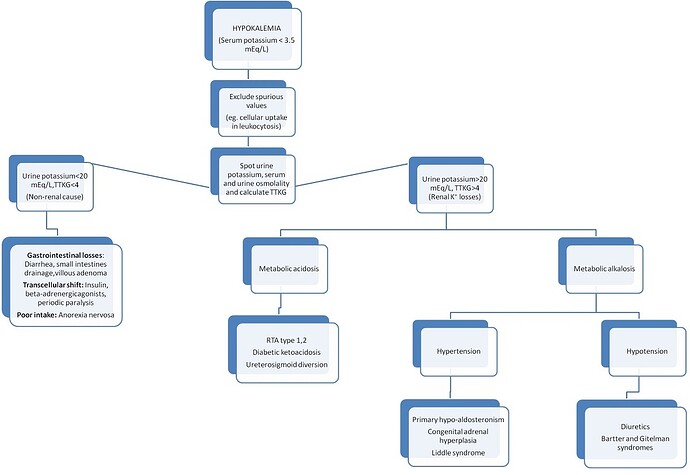
If TTKG is less than 4, it means that kidney are not wasting excessive potassium and the cause is extra-renal. If TTKG is more than 4, it means renal loss is the cause of hypokalemia.
Diagnostic approach to Hypokalemia is made as follows:
Diagnostic Approach to Hypokalemia
Treatment
Using the diagnostic approach, underlying cause is found and treated. If TTKG is less than 4, causes of GIT loss, transcellular shift and poor intake are corrected. If the TTKG is more than 4, acidosis or alkalosis is explained and corrected. Hypertension associated with metabolic acidosis generally clue towards primary hypoaldosteronism or genetic disease.
Potassium levels deficit is corrected over 24 hours, if severe hypokalemia (low potassium less than 2.5 mEq/L) or associated with cardiac arrythmia, then IV correction may be necessary.
Hyperkalemia
Hyperkalemia or increased potassium levels is defined as serum potassium levels going above 5.5 mEq/L. Major mechanisms involved are decreased losses, increased intake, extracellular shift and cellular breakdown.
Renal insufficiency, acidosis and diseases involving defects in mineralocorticoid, aldosterone and insulin are some major causes of high potassium levels.
Pseudo-hyperkalemia is caused by thrombocytosis, leukocytosis and packed red blood cells infusion.
Causes
True hyperkalemia is caused by one or more of 3 mechanisms : Increased potassium intake, extracellular potassium shifts or decreased excretion.
Following table lists the causes of hyperkalemia which includes Decreased losses of Potassium, Increased intake of Potassium, Extracellular shift of Potassium from extracellular to intracellular and Cellular breakdown.
HYPOKALEMIA CAUSES
Increased losses Renal loss: RTA (Renal tubular acidosis), Drugs like loop diuretics and thiazides, steroids, cystic fibrosis, giletman syndrome, bartter syndrome, liddle syndrome, mineralocorticoid excess (cushing syndrome, hyperaldosteronism, congenital adrenal hyperplasia), renin secreting tumors, renal artery stenosis
Extra-renal loss: Diarrhea, vomiting, sweating, potassium binding resins
Decreased intake or stores Malnutrition, anorexia nervosa; potassium-poor parenteral control
Intracellular shift Alkalosis, medications like beta-2 adrenergic agonists, theophylline, barium; refeeding syndrome, hypokalemic periodic paralysis, high insulin state, malignant hyperthermia, thyrotoxic periodic paralysis.
Signs and Symptoms
Sudden and rapid onset of hyperkalemia can result in severe cardiac arrythmia. Patients often report nausea, vomiting, parasthesias, muscle weakness, fatigue and ileus. ECG findings are significant as elevated potassium levels interfere with repolarization of cellular membrane during cardiac conduction.
These ECG changes include tall T waves, prolonged PR interval, flat P waves, wide QRS complex, absent P waves, bundle branch blocks and eventually sine waves.
Treatment
High potassium levels on sudden and rapid onset are most serious electrolyte disturbances. They promptly need to be treated. Treatment of hyperkalemia involve discontinuation of potassium-containing fluids and medications which are causing hyperkalemia. Stabilization of myocardial cell membrane to prevent cardiac arrythmia is another important step. Cellular uptake of potassium is enhanced, for which insulin and glucose, sodium bicarbonate or beta-adrenergic agonists may be used
Diuretics are used to ensure total body potassium elimination only if kidneys are not compromised. Finally, hemodialysis may be required for treatment of severe symptomatic hyperkalemia that is resistant to drug therapy with patients having impaired renal functions.