Q-1. In a case of endometrial carcinoma, external beam radio-therapy in pelvis has been planned. Which is the most radio-sensitive organ/tissue in this region of pelvis?
a) Vagina
b) Rectum
c) Ovary
d) Urinary Bladder
Answer: Ovary
Explanation:
Radio-sensitivity is the relative susceptibility of cells, tissues, organs, organisms, or other substances to the injurious action of radiation. In general, it has been found that cell radio-sensitivity is directly proportional to the rate of cell division and inversely proportional to the degree of cell differentiation.
High Radiosensitive organs/tissues:
Lymphoid organs, bone marrow, blood, testes, ovaries and intestines
Q-2. In case of dysmenorrheal and tender uterus with normal biopsy of endometrium. USG shows diffuse enlarged uterus with no adnexal mass. What is most probable cause?
a) Endometritis
b) Leiomyoma
c) Adenomyosis
d) Endometriosis
Answer: Adenomyosis
Explanation:
Adenomyosis is the presence of endometrial tissue in the myometrium of uterus and is a benign condition.
Adenomyosis can spread throughout the myometrium or can form nodules called adenomyomas.
The diagnosis is often suggested by a combination of symptoms, such as heavy bleeding and painful periods, combined with a physical examination revealing an enlarged, boggy uterus.
Q-3. A 19 years old female who has not yet achieved menarche presents with normal growth, breast development, and pubic hair. On vaginal examination, vaginal end is blind and uterus is not palpable. What is diagnosis?
a) Turner syndrome
b) Gonadal dysgenesis
c) Androgen insensitivity syndrome
d) Mullerian agenesis
Answer: Mullerian agenesis
Explanation:
Mullerian agenesis:
Mullerian agenesis patients have primary amenorrhea & absent uterus (Hence will not respond to OCPs) but have normal well developed breast, axillary and pubic hair.
Androgen Insensitivity syndrome:
X-linked recessive disorder
Karyotype XY
External genitalia look like female
Adequate breast development without axillary and pubic hair or minimal axillary and pubic hair
Primary amenorrhea and absent uterus, hence will not respond to OCPs
Testes are placed in either labia or inguinal canal, or are intra-abdominal
Q-4. During full term pregnancy, all are increased except
a) Cardiac output
b) Blood volume
c) GFR
d) Minute ventilation
Answer: Cardiac output (Most correct answer)
Explanation:
Cardiac output at rest when measured in the lateral recumbent position increases significantly beginning in early pregnancy.
Even cardiac output at term is more as compared to a non-pregnant female, but it is lesser than first and second trimester, mainly due to IVC compression.
Q-5. Double bleb sign in USG is seen in
a) Ectopic pregnancy
b) Hetero-tropic pregnancy
c) Intra-uterine two gestational sacs
d) Amniotic sac and yolk sac
Answer: Amniotic sac and yolk sac
Explanation:
Confirming intrauterine gestation:
A double bleb sign:

A sonographic feature where there is visualization of a gestational sac containing a yolk sac and amniotic sac giving an appearance of two small bubbles 2.
The embryonic disc is located between the two bubbles.
It is an important feature of an intrauterine pregnancy and thus distinguishes a pregnancy form a pseudo-gestational sac or decidual cast cyst.
Intra-decidual sac sign:
An anechoic centre surrounded by single echogenic rim surrounding gestational sac
Useful feature in identifying an early intrauterine pregnancy as early as 25 days of gestation
The double decidual sac sign:

An anechoic centre surrounded by two concentric echogenic rings surrounding gestational sac
A useful feature on early pregnancy ultrasound to confirm an early intrauterine pregnancy
It consists of the decidua parietalis (lining the uterine cavity) and decidua capsularis (lining the gestational sac) and is seen as two concentric rings surrounding an anechoic gestational sac.
Where the two adhere is the decidua basalis, and is the site of future placental formation.
Q-6. A 26 years old female presented with mild pain in lower abdomen. She has had 2 full term normal delivery earlier. Her last menstrual period was 3 weeks back. On pelvic examination, you find a palpable mass in the adnexa. On USG pelvis you find a 5 cm ovarian cyst. What should be your next step?
a) Review for cyst after 2-3 months
b) CA-125 levels
c) CECT Pelvis
d) Diagnostic laparotomy
Answer: Review for cyst after 2-3 months
Explanation:
Premenopausal females: Ovarian cyst
For simple ovarian cysts greater than 5 cm but less than 7 cm:
Wait and watch or
Oral contraceptive pills
For simple ovarian cysts greater than 7 cm:
Further imaging with MRI or
Surgical assessment
Post-menopausal females: Ovarian cyst
For simple ovarian cysts greater than 1 cm but less than 7 cm:
Yearly follow up
For simple ovarian cysts greater than 7 cm:
Further imaging with MRI or
Surgical assessment
Q-7. An episiotomy is to be performed in a primigravida in labour. Which of these is an advantage of medio-lateral episiotomy over midline episiotomy?
a) Less blood loss
b) Easy repair
c) Easy proximation
d) Less extension of tear
Answer: Less extension of tear
Explanation:
A medio-lateral episiotomy is preferred because it has a much lesser chance of extension through the perineum till anal sphincter, though there is increased risk of blood loss and it is difficult to repair.
Q-8. A 22 years 3 para 2 lady delivers a normal child followed by delivery of an intact placenta. Following delivery the lady develops severe per vaginal bleeding after 30 minutes. On table sonogram revealed retained placental tissue. What is suspected type of placenta?
a) Placenta succenturiate
b) Placenta accrete
c) Placenta fenestrae
d) Membranous placenta
Answer: Placenta succenturiate
Explanation:
Placenta succenturiate:
A succenturiate lobe is a variation in placental morphology and refers to a smaller accessory placental lobe that is separate to the main disc of the placenta.
There can be more than one succenturiate lobe.
Complications of placenta succenturiate:
Increased incidence of type II vasa previa
Increased incidence of postpartum hemorrhage due to retained placental tissue
Q-9. 25 year old female presents with complains of infertility in gynecology department. Hystero-salpingogram reveals Asherman syndrome. Clinical feature associated with Asherman syndrome is
a) Oligo-menorrhea
b) Poly-menorrhea
c) Menorrhagia
d) Hypo-menorrhea
Answer: Hypo-menorrhea
Explanation:
Asherman syndrome, also known as uterine synechiae, is a condition characterized by formation of intrauterine adhesions.
Common presenting feature of Asherman’s syndrome:
Infertility
Pregnancy loss
Menstrual abnormalities such as pypo-menorrhoea or amenorrhea
Abdominal pain
Important point:
Gold standard investigation- Direct visualization of uterine cavity by Hysteroscopy
Q-10. For what procedure, following instrument is used

a) Dilatation and curettage
b) Endometrial biopsy
c) Fractional curettage
d) Dye instillation in Hystero-salpingography
Answer: Dilatation and curettage
Explanation:
Karman cannula:
A soft, flexible cannula popularized by Harvey Karman in the early 1970s.
The Karman cannula used for:
Endometrial aspiration
Dilatation and curettage
Rubin’s cannula:
![]()
This cannula is used for tubal patency test for infertility like HSG (Hystero-salpingography) or Chromo perturbation in laparoscopy.
In HSG radio opaque iodine (Urographin) is used.
For laparoscopy Methylene Blue dye is injected through the cannula.
This cannula has a rubber guard which needs adjustment. It prevents backward leak of the dye.
Q-11. A routine ultrasound done at 20 weeks period of gestation done in a 31 year old gravida 1 para 0 revealed an anomaly as in USG film. What is congenital anomaly?

a) Cystic hygroma
b) Encephalocele
c) Omphalocoele
d) Anencephaly
Answer: Anencephaly
Explanation:
Anencephaly is the most severe form of cranial neural tube defect and is characterized by absence of cortical tissue (although brainstem and cerebellum may be variably present) as well as absence of the cranial vault.
Antenatal ultrasound features:
Anencephaly may be sonographically detectable as early as 11 weeks and has an accuracy of approximating 100 % at 14 weeks.
Less than expected value for crown rump length (CRL)
A “Frog eye” or “Mickey mouse” appearance may be seen when seen in the coronal plane due to absent cranial bone/brain and bulging orbits.
May show evidence of poly-hydramnios due to impaired swallowing
Q-12. A 30 years old primigravida presented at 10 weeks gestation with painless, bright red bleeding per vaginum. On examination the uterus is 12 weeks size. USG revealed the following findings. What is the likely diagnosis?
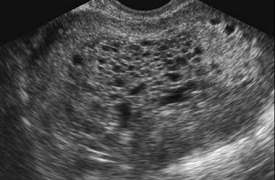
a) Blighted ovum
b) Hydatiform mole
c) Missed abortion
d) Placental polyp
Answer: Hydatiform mole
Explanation:
Hydatiform mole:
Clinical examination and beta-hCG determinations are the recommended initial tests for hydatidiform mole.
Ultra-sonography is the imaging investigation of choice to confirm the diagnosis of hydatidiform mole.
USG film demonstrates a distended endometrial cavity containing innumerable, variably sized anechoic cysts with intervening hyper-echoic material (snowstorm or granular appearance).
The molar tissue demonstrates the bunch of grapes sign which represents hydropic swelling of trophoblastic villi.
Q-13. Findings of PAP-smear taken during the late menstrual period from a 45 years old lady suffering with an ovarian tumor are as follow. What is the likely histology of tumor?
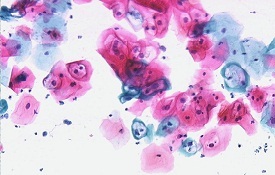
a) Granulosa cell tumor
b) Dysgerminoma
c) Serous papillary carcinoma
d) Mucinous Adenocarcinoma
Answer: Granulosa cell tumor
Explanation:
PAP smear:
The Pap smear is a screening test only. Positive tests are an indication for further diagnostic procedures.
Para-basal cells (Blue colored) are the least mature cells and not affected by estrogen.
Superficial cells (Orange colored) display the most maturity and affected by estrogen.
Important points:
When maturing, the nucleus becomes smaller and cytoplasm becomes larger.
The shape of cells becomes less round the more maturity they are.
Granulosa cell tumors commonly produce estrogen.
Q-14. A primigravida came to the labour room at 40 weeks + 5 days gestation. On per vaginal examination
Cervix 1 cm dilated
30 % effacement
Vertex at -1 station
Cervix soft and posterior
Calculate modified Bishop’s score in above case:
a) 3
b) 5
c) 7
d) 8
Answer: 5
Explanation:
Bishop Score:
Cervix: Position
Score 0: Posterior
Score 1: Mid posterior
Score 2: Anterior
Score 3: —-
Cervix: Consistency
Score 0: Firm
Score 1: Medium
Score 2: Soft
Score 3: —-
Cervix: Effacement
Score 0: 0-30 %
Score 1: 40-50 %
Score 2: 60-70 %
Score 3: > 80 %
Cervix: Dilatation
Score 0: Closed
Score 1: 1-2 cm
Score 2: 3-4 cm
Score 3: > 5 cm
Cervix: Head station
Score 0: -3
Score 1: -2
Score 2: -1
Score 3: + 1, + 2
Modified Bishop Score:
According to the Modified Bishop’s pre-induction cervical scoring system, effacement has been replaced by cervical length in cm, with scores as follows- 0 >3 cm, 1 >2 cm, 2> 1 cm, 3> 0 cm
Q-15. A 30 year G3P2 with 10 weeks of amenorrhea comes with intra-uterine pregnancy with an IUCD in situ. On pelvic examination, the string of the IUCD was visible at cervical os. Patient wishes to continue pregnancy. The most appropriate course of action is to
a) Terminate pregnancy because of high risk of infection
b) Remove IUCD
c) Leave IUCD and continue pregnancy
d) Continue pregnancy with use of antibiotics through pregnancy
Answer: Remove IUCD
Explanation:
Women with an intrauterine pregnancy with an IUD in situ should be advised to have the IUD removed before 12 completed weeks’ gestation, whether or not they intend to continue the pregnancy.
Complications of IUCD in situ during pregnancy:
Increased risks of second-trimester miscarriage
Preterm delivery
Infection