Rickets is the softening and weakening of bones in children, usually because of an extreme and prolonged vitamin D deficiency.
Vitamin D promotes the absorption of calcium and phosphorus from the gastrointestinal tract. A deficiency of vitamin D makes it difficult to maintain proper calcium and phosphorus levels in bones, which can cause rickets.
Adding vitamin D or calcium to the diet generally corrects the bone problems associated with rickets. When rickets are due to another underlying medical problem, your child may need additional medications or other treatment. Some skeletal deformities caused by rickets may require corrective surgery.
Signs and symptoms of rickets can include:
Delayed growth
Pain in the spine, pelvis and legs
Muscle weakness
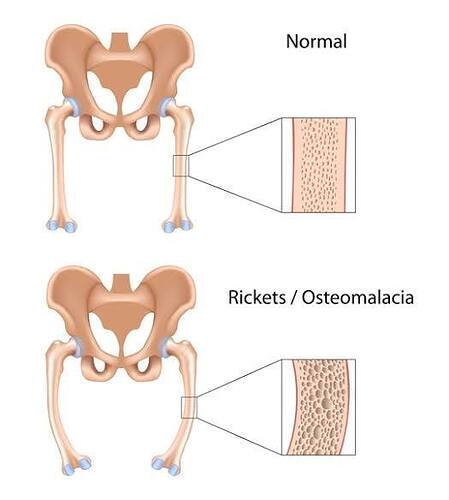
Because rickets softens the growth plates at the ends of a child’s bones, it can cause skeletal deformities such as:
Bowed legs or knock knees
Thickened wrists and ankles
Breastbone projection
When to see a doctor
Talk to your doctor if your child develops bone pain, muscle weakness or obvious skeletal deformities.
Your body needs vitamin D to absorb calcium and phosphorus from food. Rickets can occur if your child’s body doesn’t get enough vitamin D or if his or her body has problems using vitamin D properly. Occasionally, not getting enough calcium or lack of calcium and vitamin D can cause rickets.
Lack of vitamin D
Children who don’t get enough vitamin D from these two sources can develop a deficiency:
Sunlight. Your skin produces vitamin D when it’s exposed to sunlight. But children in developed countries tend to spend less time outdoors. They’re also more likely to use sunscreen, which blocks the rays that trigger the skin’s production of vitamin D.
Food. Fish oils, fatty fish and egg yolks contain vitamin D. Vitamin D also has been added to some foods, such as milk, cereal and some fruit juices.
Problems with absorption
Some children are born with or develop medical conditions that affect the way their bodies absorb vitamin D. Some examples include:
Celiac disease
Inflammatory bowel disease
Cystic fibrosis
Kidney problems
Risk factors
Factors that can increase a child’s risk of rickets include:
Dark skin. Dark skin doesn’t react as strongly to sunshine as does lighter skin, so it produces less vitamin D.
Mother’s vitamin D deficiency during pregnancy. A baby born to a mother with severe vitamin D deficiency can be born with signs of rickets or develop them within a few months after birth.
Northern latitudes. Children who live in geographical locations where there is less sunshine are at higher risk of rickets.
Premature birth. Babies born before their due dates are more likely to develop rickets.
Medications. Certain types of anti-seizure medications and antiretroviral medications, used to treat HIV infections, appear to interfere with the body’s ability to use vitamin D.
Exclusive breast-feeding. Breast milk doesn’t contain enough vitamin D to prevent rickets. Babies who are exclusively breast-fed should receive vitamin D drops.
Left untreated, rickets can lead to:
Failure to grow
Abnormally curved spine
Skeletal deformities
Dental defects
Seizures
Exposure to sunlight provides the best source of vitamin D. During most seasons, 10 to 15 minutes of exposure to the sun near midday is enough. However, if you’re dark-skinned, if it’s winter or if you live in northern latitudes, you might not be able to get enough vitamin D from sun exposure.
In addition, because of skin cancer concerns, infants and young children, especially, are warned to avoid direct sun or to always wear sunscreen and protective clothing.
To prevent rickets, make sure your child eats foods that contain vitamin D naturally — fatty fish, fish oil and egg yolks — or that have been fortified with vitamin D, such as:
Infant formula
Cereal
Bread
Milk, but not foods made from milk, such as yogurt and cheese
Orange juice
Check labels to determine the vitamin D content of fortified foods.
If you’re pregnant, ask your doctor about taking vitamin D supplements.
Because human milk contains only a small amount of vitamin D, all breast-fed infants should receive 400 international units (IU) of oral vitamin D daily.
The American Academy of Pediatricians recommends that breast-fed infants or those who drink less than 33.8 ounces (1 liter) of infant formula a day to take an oral vitamin D supplement