Diabetic foot ulcers occur in approximately 10% of patients with type 1 or type 2 diabetes mellitus. Diabetic foot ulcers are more common in patients who also have other evidence of other micro- or macrovascular disease (retinopathy, nephropathy, or coronary heart disease).

Pathophysiology
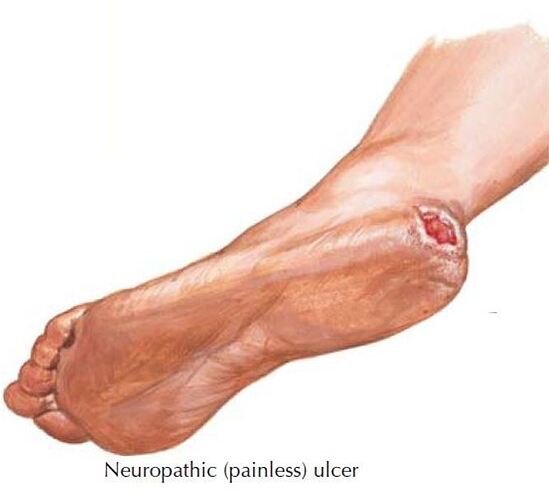
Diabetic neuropathy (see Plate 5-16) plays a key role in diabetic foot ulcers. For example, sympathetic autonomic neuropathy may result in dry skin (from decreased sweat production), leading to scaling, cracks,and fissures, which provide a portal for infection.
The prominent metatarsal heads become the point of impact of body weight and friction and a common site of diabetic foot ulcer development.
Motor neuropathy affects the small intrinsic muscles of the feet so that the larger muscles in the anterior tibia compartment are unopposed, causing subluxation of the proximal interphalangeal-metatarsal joints (claw toe deformity).
Plantar callus, which predisposes to ulceration, may build up at these high-pressure sites. The presence of neuropathy increases the risk of diabetic ulcer formation sevenfold.
How to diagnosis the diabetic foot ?
Patients with diabetes should have annual comprehensive foot examinations to assess for evidence of neuropathic or vascular deficits, deformity, callus formation, or dry skin.
bration sensation should be tested with a 128-Hz tuning fork at the great toe.
Pressure sensation should be tested with a Semmes-Weinstein 5.07 (10-g) monofilament applied to buckling pressure on the plantar surface of the foot.
the Achilles tendon reflex and temperature sensation should be checked.
Vascular insufficiency can be evaluated with assessment of pulses (dorsal pedis, posterior tibia), skin temperature, presence of hair on skin, color of skin, and assessment for dependent rubor.
How to prevent for the diabetic foot ulcer?
Prophylactic measures to prevent diabetic foot ulcers include smoking cessation; avoiding walking barefoot; checking water temperature before stepping into a bath; keeping the toenails trimmed; inspecting the feet daily for blisters, swelling, or redness; and wearing properly fitting shoes.
Classification of Diabetic foot ulcer
The Wagner diabetic foot ulcer classifi cation scheme is as follows:
Grade 0: No ulcer but high-risk (e.g., deformity, callus, insensitivity)
Grade 1: Superficial full-thickness ulcer
Grade 2: Deeper ulcer that penetrates tendons but does not involve bone
Grade 3: Deeper ulcer with bone involvement (osteitis)
Grade 4: Partial gangrene (e.g., toes and forefoot)
Grade 5: Gangrene of the whole foot



Investigation
Key steps to ensure effective healing of diabetic foot ulcers include confirming adequate arterial blood flow, treating underlying infection, removing pressure from the wound and surrounding area, and debriding all dead and macerated tissue.
A nonhealing foot ulcer should be investigated for ischemia with noninvasive techniques and arteriography in some cases.
If osteomyelitis is suspected, additional imaging is indicated with a combination of plain radiographs, magnetic resonance imaging, and bone scintigraphy.
Therapy for diabetic foot ulcer
The treatment of osteomyelitis requires systemic antibiotic therapy and, in many cases, surgical removal of infected bone.
Localized gangrene of a toe that is not associated with infection may be allowed to self-amputate.
Extensive gangrene is a medical urgency that requires hospitalization, treatment of the underlying infection, optimizing glycemic control, vascular assessment, and consultation with vascular and orthopedic surgeons.